A robust safety profile in AS that is tried through 5 years
AS safety profile through Week 16 and Year 1: MEASURE 1 and 2 (pooled data, any dose)1,2*
AEs ≥2% and higher than placebo | COSENTYX® (n=394), % | Placebo (n=196), % |
Nasopharyngitis | 11.2 | 6.1 |
Upper respiratory tract infection | 2.5 | 2.0 |
Nausea | 3.8 | 2.6 |
Selected AEs through Week 161,2* | COSENTYX (n=394), % | Placebo (n=196), % |
Infections | 31 | 18 |
Serious infections | 0.3 | 0 |
If a serious infection develops, discontinue COSENTYX until the infection resolves1
If an anaphylactic reaction or other serious allergic reaction occurs, discontinue COSENTYX immediately and initiate appropriate therapy1
Evaluate patients for TB prior to initiating treatment1
Incidence of inflammatory bowel disease1* | 16-week period | After 16-week period and up to 52 weeks | Entire treatment period (≥52 weeks) |
Crohn’s disease | 2 exacerbations | 1 new onset and 2 exacerbations | 0.7 (5 cases) |
Ulcerative colitis | 1 new onset | 1 new onset and 1 exacerbation | 0.4 (3 cases) |
Adverse reactions reported by >1% of patients in clinical trials for moderate to severe PsO were nasopharyngitis, diarrhea, upper respiratory tract infection, rhinitis, oral herpes, pharyngitis, urticaria, and rhinorrhea.1
AS safety profile through Year 5
MEASURE 2 (n=211) | ||||
COSENTYX any dose, | Year 24 | Year 35 | Year 46 | Year 57 |
Serious infections | 1.2 | 1.5 | 1.5 | 1.8 |
Candida infections | 0.9 | 1.0 | 1.2 | 1.0 |
Crohn’s disease | 0.7 | 0.6 | 0.6 | 0.5 |
Ulcerative colitis | 0.7 | 0.6 | 0.4 | 0.4 |
IBD unclassified | 0.2 | 0.2 | 0.1 | 0.1 |
MACE | 0.5 | 0.6 | 0.6 | 0.6 |
Malignancy | 0.5 | 0.6 | 0.4 | 0.6 |
EAIR is defined as the number of patients with a particular AE divided by the total exposure time among patients in the respective treatment group at risk of an initial occurrence of the event.8
Background rate: According to a pooled estimate from a meta-analysis across 69 articles and ~32,000 patients‡ with AS, 6.8% had IBD (95% CI: 6.1%, 7.7%; I2=84.2%). These studies did not specifically assess COSENTYX.9
~99.4% had NO immunogenicity over 5 years10
Neutralizing antibodies developed in approximately 0.6% of patients with PsO and were not associated with loss of efficacy10||
Please see Important Safety Information, including CONTRAINDICATIONS.
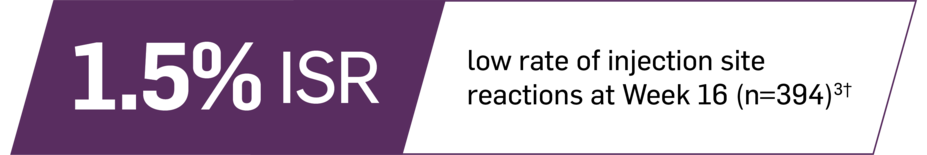
†Rate of injection site reactions means the percentage of patients affected by 1 or more injection site reactions during the first 16 weeks of the pooled MEASURE 1 and 2 trials, respectively.3
‡7% (n=2251) had a history of IBD.
§All trials used SC administration.
||The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors, including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease.
Definitions
AE, adverse event; AS, ankylosing spondylitis; EAIR, exposure-adjusted incidence rate; IBD, inflammatory bowel disease; IV, intravenous; MACE, major adverse cardiovascular event; PsO, plaque psoriasis; PY, patient-year; SC, subcutaneous; TB, tuberculosis.
References
1. Cosentyx. Prescribing information. Novartis Pharmaceuticals Corp.
2. Data on file. AIN457H Summary of Clinical Safety in Ankylosing Spondylitis. Novartis Pharmaceuticals Corp; February 2015.
3. Data on file. AIN457F Summary of Clinical Safety Appendix 1. Novartis Pharmaceuticals Corp; February 2015.
4. Data on file. Selected EAIRs MEASURE 2 Year 2. Novartis Pharmaceuticals Corp; January 2020.
5. Data on file. Selected EAIRs MEASURE 2 Year 3. Novartis Pharmaceuticals Corp; January 2020.
6. Data on file. Selected EAIRs MEASURE 2 Year 4. Novartis Pharmaceuticals Corp; January 2020.
7. Data on file. Selected EAIRs MEASURE 2 Year 5. Novartis Pharmaceuticals Corp; January 2020.
8. Data on file. CAIN457H2315 (PREVENT): Clinical Study Report. Novartis Pharmaceuticals Corp; November 2019.
9. Stolwijk C, van Tubergen A, Castillo-Ortiz JD, Boonen A. Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: a systematic review and meta-analysis. Ann Rheum Dis. 2015;74(1):65-73.
10. Reich K, Blauvelt A, Armstrong A, et al. Secukinumab, a fully human anti-interleukin-17A monoclonal antibody, exhibits low immunogenicity in psoriasis patients treated up to 5 years. J Eur Acad Dermatol Venereol. 2019;33(9):1733-1741.
11. Data on file. CAIN457F2310 (MEASURE 2): Clinical Study Report. Novartis Pharmaceuticals Corp; November 2014.
12. Data on file. CAIN457F2310 (MEASURE 2): Data Analysis Report. Novartis Pharmaceuticals Corp; June 2019.